“I want you to have the best relationship with food possible. Let’s break through the nutrition noise and find a life where all food is good food. I help people recover from eating disorders and heal your relationship with food.”
Priya Tew, Specialist Dietitian and Nutritionist BSc, PG Dip, MSc


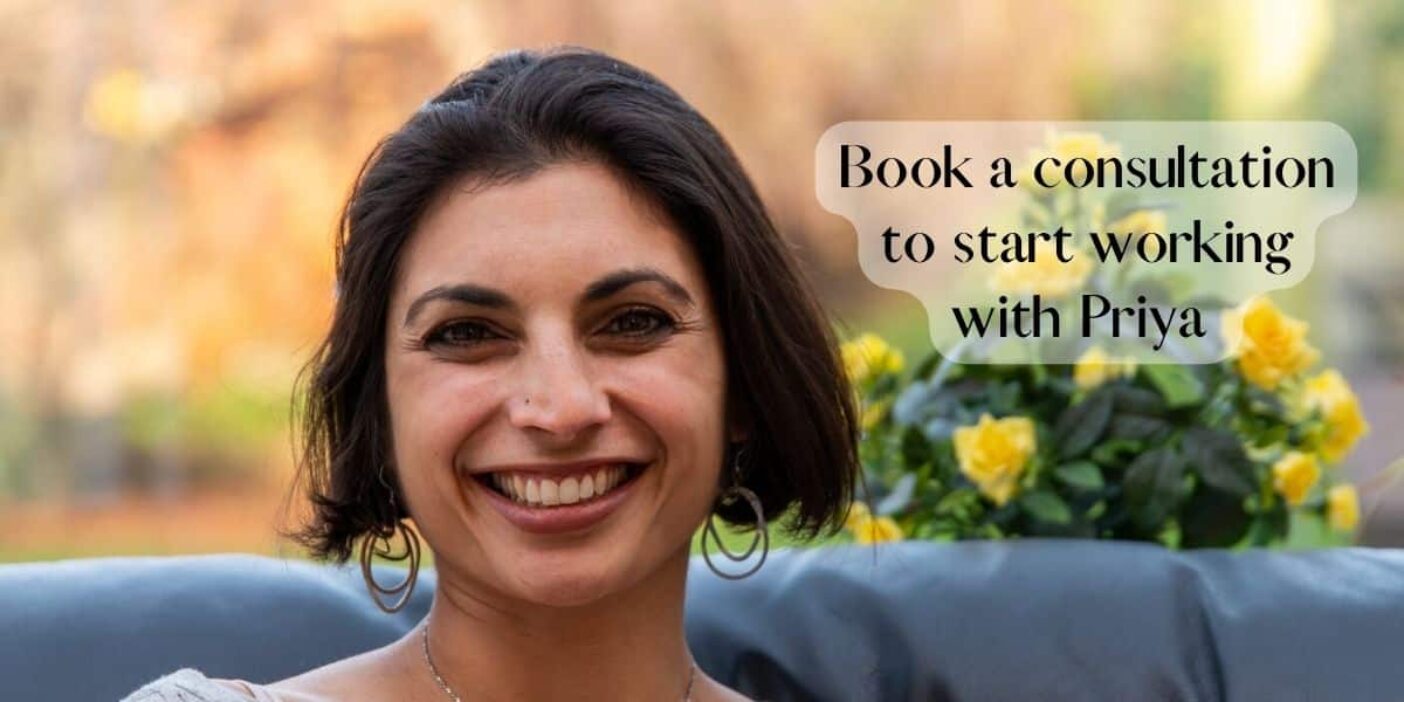
Hi, I’m Priya
I’m the dietitian who wants to help you heal your relationship with food and throw away those scales. I’ve worked in eating disorders for longer than I want to say (okay, it’s been almost 25 years) and seen every diet and trick in the book. It still devastates me to see the impact disordered eating can bring.
Food to me, is so much more than just nutrition and weight. It can bring joy and makes occasions special (think birthday cake).
Yes, I can help you plan what and when to eat, but what I really love to do is dig into the psychology of eating. With my wealth of experience and training I can do just that. I’m not just an eating disorders dietitian, I’m the one that can help you break this cycle for life.

“Words cannot explain how amazing Priya has been throughout my ED recovery. Seeing a dietician felt really daunting, but Priya put me at ease instantly. She is so kind, empathetic and patient.<br>I started seeing Priya because I was struggling with both orthorexia and anorexia. At the start of my recovery journey, I was terrified of food and I felt so depressed. I thought my relationship with food was irreparable, but Priya changed that.<br>She has such extensive knowledge of food and eating disorders. I had so many fear foods and food rules, but Priya has helped me to challenge these. And I now eat foods that I never I thought I would eat again. And enjoy them!”

“We were recommended Priya a couple of years ago when we needed specialist advice and support for our daughter who had been diagnosed with Anorexia. Priya is incredibly knowledgeable in her field and was just what we needed at a time we felt completely out of our depths and very anxious. Priya was kind and empathic and supported us in so many ways at the beginning of our daughters recovery. The insights, awareness, advice and guidance she gave us all was extremely valuable. Priya was always realistic and encouraged us to remain hopeful, reminding us that recovery is possible. We now know it is. We will be forever grateful. Don’t hesitate to contact Priya if you or a loved one is struggling.”

“Recovery is challenging, but having the support of Priya has made all the difference. She has been so reassuring, and I have learnt so much from her. I am incredibly grateful to her and always will be.
I continue to see Priya as I work through my recovery, but I have come such a long way already. My world is so much bigger than it was, and the eating disorder voice is getting quieter. If you are struggling with your relationship with food, I cannot recommend Priya enough. Let her help you to live the full life you deserve.”
Collaborations
The Flexible Eating Course
Find out about my 6-week course where you’ll learn to eat more flexibly and how to embrace your health for life. This is not about weight loss but about a healthy relationship with food and your body
Books by Priya
Have a look at my two books, The Dash Diet, and The Complete Low FODMAP Diet Plan available to buy online and in stores
Book A Consultation
If you’re struggling with an eating disorder and would like my support, book a consultation and start your journey towards recovery
As seen in