Continuous glucose monitoring is something that is almost becoming a trend right now. This is where you wear a device and monitor your blood sugar responses. The aim is to eat less foods that cause large spikes in blood sugars to look after your long term health. However is this actually a trend you need to follow?
In this blog we are going to look at:
- What happens to blood glucose levels when we eat?
- What is a CGM?
- What is type 2 diabetes?
- Do I need to monitor my blood sugars?
- Are low blood sugars healthy?
- What are the risks of continuous glucose monitoring?
How do I track blood sugar levels with continuous glucose monitoring?
Monitoring blood sugar levels has become increasingly popular in recent months. This is as part of biometric trends to hack your way into optimal health. This is occuring especially via app-friendly devices like continual blood glucose monitors (CGM). Let’s just be clear that is it perfectly normal for your blood sugar (glucose) levels to rise after you eat. This is how the body is designed to work. When your blood sugars increase after eating food, it triggers insulin to be released. Insulin plays a critical role, it helps glucose to enter our cells, where it can be used as energy, or be stored for later.
The glucose can be used straight away as energy to fuel the body and the brain. (Did you know the brain needs glucose to function? Low levels can impair how you think and make decisions). Excess glucose can be stored in the liver or the muscles as glycogen. Then, when there is not enough blood glucose, a hormone called glucagon is released. This is to signal for glycogen to be broken down and used as energy.
Factors like stress, sleep and exercise can impact blood glucose as well. Remember, these fluctuations are a normal part of our bodies functioning and mean we don’t need to eat constantly!
What is continuous glucose monitoring? (CGM’s)
Continuous glucose monitoring involves using CGMs, a wearable device that tracks your blood glucose. These devices are designed to give a consistent and live track of blood sugar levels. This maps the rise and fall of your blood sugars throughout the day. CGMs have in part replaced traditional finger pick tests. They were designed to help monitor when and how much insulin to administer. As well as alert for any extreme highs and lows in levels of blood glucose.
You may have noticed someone wearing a CGM on the back of their arm. They can look like a round patch and they are often white. CGMs are made up of 3 parts:
- A small sensor sits just under the skin which measures your blood sugar levels.
- A transmitter is attached to the sensor and sends the readings to a device.
- A device such as a mobile phone is able to show the results.
These devices are designed for people with diabetes who use insulin. But do you need to use one yourself?
Tracking blood glucose levels has become a popular method to adjust diet and lifestyle to try to get healthier. CGMs have become the must-have gadget to show your commitment to the trend. The belief is that using CGMs to minimise your glucose spikes will reduce your risk of lifestyle diseases. This includes type 2 diabetes.
What is type 2 diabetes
Type 2 diabetes is a disease caused by the body becoming increasingly resistant to insulin. It doesn’t mean insulin is not produced, more the body doesn’t listen to it. This means that the body has to produce more and more insulin to manage the same amount of glucose. The causes for type 2 diabetes are complex. Family history and ethnicity are two of the biggest risk factors for diabetes -two factors outside of your control. One of the biggest misconceptions about diabetes is that it is caused by eating too much sugar. However, diet is more likely to increase your diabetes risk due to its long term health impact rather than the day-to-day blood glucose variability.
Do I need to monitor blood sugar levels
Monitoring blood glucose may be useful for someone at risk of developing diabetes. For example, someone with a strong family history of type 2 diabetes. Or someone who has a high HbA1c (average blood sugar levels) reading. In these examples, tracking blood glucose may help to identify what is causing too much of an increase in blood glucose levels.
However, for the typical person, tracking blood glucose isn’t needed. The rises and fall in glucose levels are a normal part of our bodies’ physiology. Most people don’t experience extreme spikes or lows in blood glucose levels. Our insulin production is able to manage the day to day variations.
Sometimes monitoring your blood sugars may be useful if you are training for an event, or for certain health conditions. The general person is unlikely to need to do this and it can actually lead to anxiety over food and cutting out food groups.
Is a food healthy if it increases blood sugar?
The problem with relying on CGMs as a marker of health, or trying to reduce blood glucose changes, is that it is an incomplete marker of health. All foods containing carbohydrates can increase glucose levels in one way or another. We need these carbohydrate foods in our diets for energy, fibre and health. Many carbohydrate-containing foods are associated with positive health outcomes. For example eating wholegrains provide fibre for our digestive health, are good for our heart health too and provide B vitamins, minerals and antioxidants. In contrast, a food high in fat but low in carbohydrate such as butter, oil or even processed meat, won’t increase blood glucose levels much, but we wouldn’t suggest only eating these foods. Balance as ever is key to our diets.
Are low blood sugars healthy
Too much focus on low blood sugars can cause unnecessary food anxiety. It can demonise health-promoting foods and doesn’t have any evidence of reducing diabetes or heart disease risk. In fact, replacing veggies and sources of fibre with saturated fats could increase you cardiovascular disease risk. If tracking blood glucose levels causes you to choose more energy-dense foods, your dietary intake may shift away from one that suits your body’s needs.
Keeping blood sugar levels as low as possible isn’t healthy. For starters, going very low could mean your cells aren’t getting enough energy. Think about the way you feel when you are very hungry. You might have wobbly legs, feel light headed or like you’re going to faint. These are all signs that your blood glucose levels are too low!
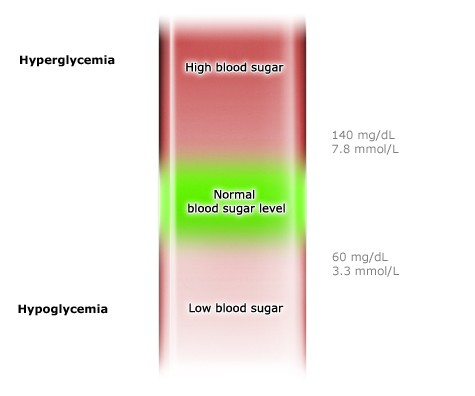
But even if you’re trying to just reduce the peaks of your blood sugar; is this healthy? Slight fluctuations are completely normal, and trying to stop little rises in blood glucose will have no benefit. There’s not even necessarily a strict cut off for what we count as normal or healthy vs not. As you can see from the image below, there’s more of a gradient between what we count as good and bad.
Risks of tracking with continuous glucose monitors
- Unneeded Food Anxiety:
Tracking your blood glucose levels without medical need or a bigger-picture view of health, could negatively impact your eating habits and damage your relationship with food. Transient glucose spikes are brief and normal responses to eating food. Certain foods, meal compositions or simply larger meals may cause a larger increase in glucose levels than other foods. This doesn’t mean these foods are bad for you.
2. Lack of scientific research:
The current trend for tracking and lowering levels of glucose comes with lots of misinformation. There are claims that avoiding blood glucose spikes can reverse PCOS, reduce cardiovascular disease and type 2 diabetes risk, but the evidence simply isn’t there. Although extreme or prolonged highs in blood sugars aren’t necessarily healthy, transient increases that come back down again are a normal part of our physiology. Variations in glucose are normal and a part of how our bodies manage digestion and energy needs.
3. Replacing Foods can negatively impact your diet:
More concerning are the fringe claims that blood glucose tracking shows that vegetables and wholegrains are unhealthy and should be replaced by products high in saturated fats. This goes against decades of thorough and robust research. Ignoring this well-supported dietary advice could (ironically!) put you at higher risk for lifestyle diseases, especially heart disease.
The bottom line on tracking blood sugars
When we eat carbohydrates, our blood sugars rise. Insulin is then secreted to reduce these levels, by taking glucose into cells. In healthy people, glucose levels decrease. This leaves the energy from glucose available to be used steadily until the next meal. Different foods and lifestyle factors will impact how quickly these levels rise and fall. There is very limited evidence to suggest that overly managing blood glucose has any protective effect against diabetes in people who have not been diagnosed with pre diabetes.
Sugar does not cause type two diabetes. Small blood glucose spikes do not cause type two diabetes. The average person has no need to track glucose levels, especially not via a CGM.
Get expert support with diabetes, understanding blood sugar balance and diet support by booking a consultation with the Dietitian UK team. Elle is best placed to help you due to her expertise in this area.